The Stop TB Partnership, an organization managed by the United Nations Office for Project Services (UNOPS), released the “Global Plan to End TB, 2023-2030″ (hereinafter “Global Plan”) on August 16, 2022. The Global Plan to end TB, a major public health challenge, by 2030, focuses on outlining the priority actions and estimated funding needs required to end tuberculosis by 2030.
Figure 1. Cumulative resources needed for scaling up TB care and prevention, 2023–2030 (in US$ billion)
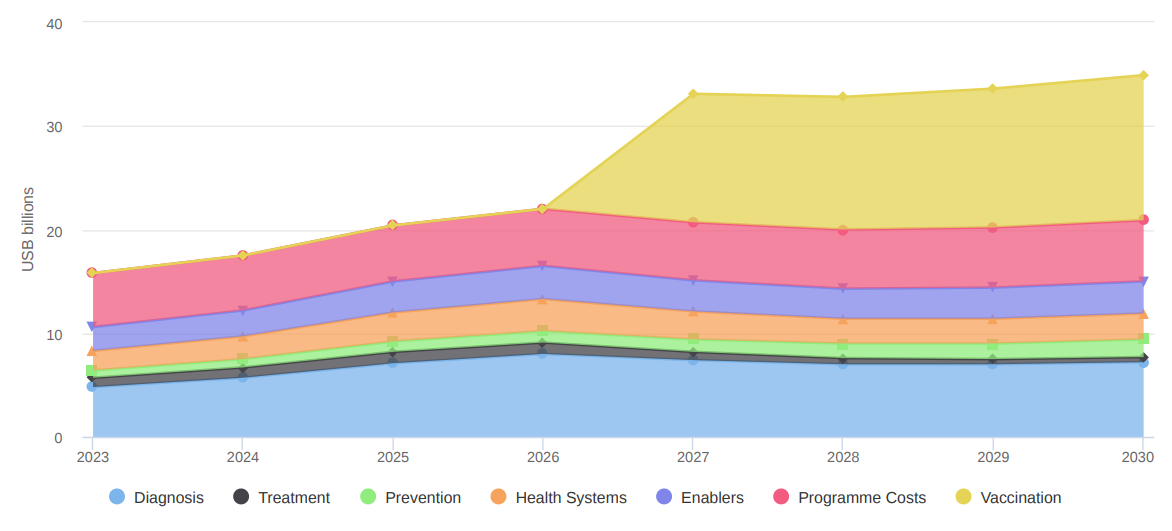
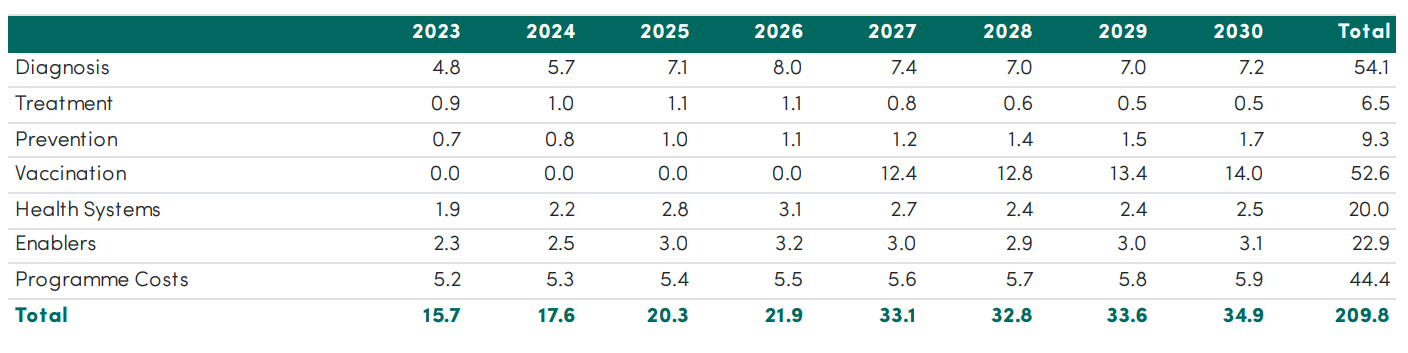
Table 1. Resource needs by cost category (US$ billions)
Note: The United Nations Office for Project Services (UNOPS) is the project management resource center of The United Nations (UN), dedicated to the implementation of the UN, international multilateral organizations and financial institutions, member governments and other international project management, international procurement services, infrastructure construction, social responsibility investment, innovation and other capacity building activities of partner institutions.
The Stop TB Partnership was established in 2001 and was previously affiliated to the World Health Organization (WHO). After 2014, it was changed to the management of the UNOPS, and is committed to leading the global campaign to end TB.
ACTION PLAN
This edition of the Global Plan consists of nine chapters. Similar to previous editions, this Global Plan emphasizes the need for political commitment and a people-centered approach to ending TB, with increased emphasis on making prevention a public health priority, while achieving universal access to TB care and support, accelerating TB research and development (R&D), introducing and scaling up novel TB tools.
CHAPTER 1 provides the international context that informs the Global Plan.
CHAPTER 2. Ending TB through comprehensive investment packages implemented at scale
CHAPTER 3. Scaling up TB diagnosis and care
CHAPTER 4. Scaling up TB prevention
CHAPTER 5. Partnering with key stakeholders: communities and the private sector
CHAPTER 6. Ending TB through universal health coverage, pandemic preparedness and response, and socioeconomic actions
CHAPTER 7. Human rights, stigma, gender, and key and vulnerable populations
CHAPTER 8. Accelerating development of new TB tools
CHAPTER 9. Resource needs, return on investment, and cost of inaction
The global situation of TB prevention and control is not optimistic, and the progress of TB prevention and control has stagnated or even regressed due to the impact of COVID-19. However, during the COVID-19 period, the capabilities of molecular diagnostic testing in many countries are improving, which makes the end of the TB epidemic with the help of molecular diagnostic platforms feasible.
SCALE UP THE USE OF MODERN DIAGNOSTICS
Millions of tuberculosis patients go undiagnosed each year, leaving patients without access to timely and effective treatment, which poses potential public health safety risks. TB diagnosis, treatment, prevention, and control are closely linked. Early detection, diagnosis, and treatment can prevent the spread of tuberculosis.
1 Universally replace sputum microscopy with rapid molecular diagnostics as the initial diagnostic test
Rapid and accessible TB diagnosis is the first step in providing effective treatment and saving lives. Many countries today still rely on sputum microscopy as the initial diagnostic test for TB. Rapid molecular tests need to replace sputum microscopy as the initial diagnostic test.
Diagnostic testing also needs to move to the point of care. This will make testing more accessible and will reduce the time it takes for people to obtain their test results and start treatment.
2 Use complementary technologies and methods to improve rapid TB detection
TB is the leading cause of death among people living with HIV (PLHIV), but it is more difficult to diagnose PLHIV using sputum. Urine-LAM is a rapid point-of-care test (usually dipstick) based on the detection of lipoarabinomannan (LAM) in urine samples, which is an easy way to detect TB infection in PLHIV. WHO recommends the test for all PLHIV with TB symptoms, regardless of their CD4 count, in both inpatient and outpatient health care settings. TB LAM should be added to diagnostic algorithms, to be used in addition to rapid molecular tests that use sputum.
Detecting TB in children has historically been challenging because of how difficult it can be for children to produce a sputum sample. In 2020, WHO recommended using stool to test for TB in children, using rapid molecular tests. This is an easy and pain-free method for rapidly testing for TB in children. It should be universally implemented.
Access to universal drug susceptibility testing (DST) is essential for successfully diagnosing and treating people with DR-TB. DST needs to become more routine and comprehensive, so that no person receives medicines to which their TB organism is resistant. This is especially important in light of WHO treatment guidelines that emphasize the use of newer medicines and treatment regimens for treating people with RR- and isoniazid-resistant TB. DST laboratory capacity and specimen referral networks need to be built to achieve this.
A chest X-ray can rapidly identify people who should receive diagnostic testing for TB. It can also reduce the number of symptomatic people requiring rapid molecular tests, along with the associated costs. CAD tools use AI to read chest X-rays for signs of TB and issue findings. These findings are then used for screening and triage.
Scaling up modern diagnostics involves more than adopting new technologies. The effort must consider the entire diagnostic network, installing new testing sites and replacing old tests in the right places to ensure people’s access.
3 Find the missing people with TB
TB can be diagnosed, treated and cured. Yet a large proportion of people developing TB are unable to access good-quality diagnosis and treatment. Such individuals are often referred to as the “missing people” with TB.
The large number of people who are missing from TB care is one of the main reasons that TB incidence and mortality have declined so slowly in recent years.
The Global Plan recommends that, at minimum, 95% of people developing TB each year need to be diagnosed and treated. Finding the missing people with TB also means ensuring that people everywhere have access to modern TB diagnostics. Old TB diagnostics such as sputum microscopy should not be used for diagnosing TB because they fail to detect 40% of TB and cannot detect drug resistance.
4 Expand early diagnosis, including at sub-clinical stages
Prevalence surveys have consistently found that about half of people with laboratory-confirmed TB do not report symptoms or are asymptomatic, which is referred to as “subclinical TB”. Knowing this, the Global Plan recommends that high TB burden countries invest significantly more resources in TB screening and active case finding aimed at detecting TB early and initiating early treatment. Populations with high rates of TB should be periodically screened for TB, regardless of symptoms.
Subclinical TB can be diagnosed by X-ray followed by bacteriological confirmation. Several initiatives have demonstrated the value of population-level TB screening followed by confirmatory molecular tests in those with abnormal X-rays.
5 Integrate TB screening and testing into other health services
Integrated service delivery (ISD) combines multiple interrelated health services in one interaction. By addressing multiple health issues simultaneously, ISD promotes convenience in ways that align with the goal of delivering people-centred care. If used widely, this approach has the potential to accelerate the finding of missing persons with TB, while addressing other health conditions that contribute to TB morbidity and mortality (i.e., HIV, diabetes, undernutrition, tobacco use, and COVID-19).
THE GLOBAL PLAN TO END TB, 2023–2030: TARGET SETTING
At least 95% of estimated TB burden should be found and 90% of those initiated on treatment should be successfully treated:
- 50.0 million people with TB in the period 2023–2030.
- 4.7 million children with TB in the period 2023–2030.
- 2.2 million people with RR- or MDR-TB in the period 2023–2030.
More than 90% of pulmonary TB should be diagnosed by rapid molecular tests, and more than 90% of bacteriologically identified TB strains should have DST before initiating treatment.
ZEESAN TB DIAGNOSTIC SOLUTIONS FACILITATES END TB INITIATIVES
ZEESAN has been involved in the field of molecular diagnostics of tuberculosis for decades. It possesses intellectual property rights of Multicolor Melting Curve Analysis (MMCA®). ZEESAN has launched the high-throughput MeltPro® TB integrated detection system and the Sanity®2.0 Fully Automated Medical PCR Analytical System. As the market leader of molecular diagnostics of tuberculosis in China, ZEESAN provides the full range of solutions covering tuberculosis screening, mycobacterial identification, drug susceptibility, personalized medication, strain traceability, etc., to provides a great boost to the rapid diagnosis of mycobacteriosis.
Rapid diagnosis is essential for effective control of drug-resistant TB outbreaks. At present, ZEESAN offers drug-resistance detection workflow covering first-line and second-line anti-tuberculosis drugs. Among them, there are 6 kits, which are CE certified, to test drug-resistance mutations involving the following drugs: rifampicin, isoniazid, fluoroquinolones, ethambutol, streptomycin and second-line injectable drug. With above capabilities, ZEESAN offers the widest range of drug-resistant TB molecular detection solution in the market.
Jan 16,2023

